Table of Contents
The months leading up to medical school graduation are exciting, but also the beginning of the next chapter: The Match.
I’m Dr. Amar Mandalia. I’ve been through The Match myself, I’ve served on admissions committees, and I’ve helped hundreds of students find success in residency applications, so let me guide you through this process.
Applying to a medical residency through the match process requires lots of forethought and planning, but this complete guide does the heavy lifting for you. We’ll help you know when to do what, plus tips from experts.
The MedSchoolCoach team and I created this guide on applying and matching to help medical students understand how to apply to residency training programs accredited by the Accreditation Council for Graduate Medical Education (ACGME) and ultimately get matched. Keep reading to learn more.
Did you know: ⅕ of all applicants don’t match into a PGY-1 position, but 97% of our clients do.
What Is the Residency Match Process?
The Match is an algorithm that takes an applicant’s rank order list (ROL) of preferred residency programs and compares them to the ROLs that programs have created to rank the applicants. The algorithm pairs these together, taking every applicant and program into consideration at the same time to place students on Match Day.
Prior to the Match, programs would individually extend offers to med students as early as their second or third year. The former process became highly competitive and much less fair.
The Nobel Prize-winning algorithm-driven Match process was invented in the 1950s to standardize the process in medical students’ fourth year and improve outcomes for both students and the program.
How It Works
After completing interviews at residency programs, med student applicants submit a rank order list (ROL) of their preferred programs to the NRMP. Meanwhile, residency programs submit a ROL of their preferred applicants.
Then, the Match algorithm goes to work. It first attempts to match applicants to their first-choice residency program at the top of their rank order list (ROL).
If the program has also ranked the applicant on their ROL and if there are open spots in the program that haven’t already been filled by applicants ranked higher by the program, then a tentative match occurs. (A tentative match means that the applicant will attend the program unless they are later displaced by the algorithm to make space for another applicant ranked higher by the program.)
If the applicant’s first-choice program hasn’t ranked them on their ROL or if all the program’s spots are already filled by higher-ranked applicants, then the algorithm will move on to the applicant’s second-choice program.
This process continues until the algorithm finds a tentative match or the applicant’s program list is exhausted.
In the latter case, the applicant does not match into a program and will have to utilize the Supplemental Offer and Acceptance Program (“SOAP”) process to find graduate medical training.
Related Read on Residency: Average Residency Salary by Specialty + Job Level
In the case of a tentative match, this becomes finalized as long as the applicant isn’t displaced by another higher-ranked applicant later in the process.
Once all applicants have either been matched or have had their ROLs exhausted, the Match process is over.
To learn more about how to make the best use of this matching algorithm for your specific circumstance, check out this helpful video on using the Residency Explorer tool by the AAMC:
ERAS Timeline
Most residency positions are offered through the Electronic Residency Application Service (ERAS). The timeline each year varies, but it generally starts in June, culminates with The Match in March of the following year, and the ERAS cycle officially ends in May.
The 2025-2026 ERAS Residency Timeline, according to AAMC.org, are:
| June 4, 2025 | ERAS 2026 season begins at 9 a.m. ET. You can now gain access to MyERAS. |
| Sept 3, 2025 | You should have fine-tuned your application well before this date and started your interview prep. Residency applicants may begin submitting MyERAS applications to programs at 9 a.m. ET. |
| Sept 24, 2025 | Residency programs are allowed to start reviewing MyERAS applications and MSPEs in the PDWS at 9 a.m. ET. |
| Mar 16, 2026 | Match Week begins, and students will be informed as to whether or not they matched to a residency program. |
| Mar 20, 2026 | The final day of Match Week, known as Match Day. |
| May 31, 2026 | ERAS 2024 season ends at 5 p.m. ET. |
Programs typically start reviewing applications at the end of September into early October. Interviews are conducted from October through February.
The Main Residency Match occurs over the process of one week in March, known as Match Week, peaking on Match Day — Friday, March 20, 2026.
Match applicants are notified the Monday of Match Week to let them know if they matched or not, but they are not given specifics on where they match. If you find out on Monday that you did not match, there’s more work to be done. You’ll need to work through the Supplemental Offer and Acceptance Program (SOAP) to find graduate medical training.
SOAP is great… but only for cleaning! Get 1-on-1 residency application advising & boost your Match odds to 97%.
Match Program Outliers
While most programs operate through ERAS and The Match, I know several programs operate outside of this structure or alongside it:
- The Military Match: Applicants in the military must complete a rank order list (ROL) and submit an application to the Joint Service Graduate Medical Education Selection Board (JSGMESB), which is in charge of the match for military-run residencies. Military medical students may also apply for civilian residencies through ERAS but are still required to submit an application and ROL to the JSGMESB, who ultimately decide whether they will be allowed to train in a civilian setting. The timeline for the Military Match is shorter than for ERAS – the application deadline is usually October 15th, and results are released on December 15th.
- The Urology Match: Certain applicants interested in urology apply through ERAS, and rank lists are due in early January. Some programs use NRMP, and some use a urology match program. Match Day is towards the end of January or early February each year.
- Ophthalmology Match: Applicants looking to go into ophthalmology apply through the Central Application Service (CAS) and match through the SF Match in January or early February.
- Preventive Medicine: Certain applicants who want to work in preventive medicine must contact individual programs to determine their process. Some use ERAS, and some use a unique application service. Many use a separate matching service outside the NRMP called the Standardized Acceptance Process (SAP). The SAP deadline for rank lists is around January 23rd. Match Day is around February 5th.
What’s Included in the ERAS Application?
Applicants should prepare their ERAS application well before the submission date in early September. The application consists of the following:
- Personal and biographical information
- Experiences
- Personal statement
- Publications
- Letters of recommendation (LORs)
- Medical Student Performance Evaluation (MSPE or “Dean’s Letter”)
- Medical school transcript
- ECFMG Status Report (for international medical graduates only)
- A photograph (optional)
- USMLE or COMLEX-USA transcripts
Get a free copy of our Complete Guide to Residency Applications.
Personal and Biographical Information
This is your basic demographic information and identity information. There is also a section for your NRMP match ID, which you will receive when you register for the NRMP Match.
If you have not registered for the NRMP Match, you can add this information later.
Experiences
This section details activities outside of your grades, similar to the Works & Activities section you filled out when applying to medical school. Use this to share who you are as a prospective student in a residency program, highlighting the qualities, skills, and interests that define your unique motivations and passions.
These experiences may range from shadowing a doctor to military service to volunteer work (and everything in between!).
You may enter up to 10 experiences, three of which can be identified as “most meaningful.” Experiences must be classified by types, and there are mission-focused characteristics to choose from per experience. There are description fields you may use for three parts of each experience: roles, responsibilities, and context.
Consider that most applicants will have similar activities, and you are trying to stand out. For this reason, use these descriptive section options to be reflective and highlight the unique aspects of your experiences (rather than just reporting the exact specifics of what you did and nothing else).
There is also a newer section called “Impactful Experiences.” Not every student should fill this out; only use it if you faced significant hardships and challenges on your way to residency.
My team wrote a comprehensive article on how to fill out the ERAS activities section — I highly recommend you read it thoroughly to utilize this section of your application.
Personal Statement
I encourage you to start writing your ERAS personal statement as far in advance as possible. When you know you want to be in a particular specialty, even if it is halfway through your second year, go ahead and start then.
Don’t wait until the application season to start your personal statement.
What do you include in a personal statement? Describe why you want to pursue your residency of choice and what will make you exceptional at it. Explain how you are uniquely qualified to serve in the medical field.
Pro tip: Keep a note on your phone or computer with notes about experiences from medical school you want to include in your personal statement. These notes can help you clarify and remember important points that will eventually go into the official essay.
ERAS allows for a personal statement about 5 pages long, but you should aim for no more than a page. Admissions committees want brevity — I’ve heard that some will stop reading after the first page, so don’t make it longer than that.
Also note that one page in word processing software is not the same thing as one page in ERAS. A one-page essay in Microsoft Word or Google Docs might appear as one and a half pages when copy-pasted into ERAS. Make sure to preview your ERAS application before submitting to avoid spilling onto the second page.
If you will be applying to more than one specialty, you’ll need a separate personal statement for each program. You will have the option during submission to assign a specific personal statement to each program.
Writing a strong personal statement starts with structure. A clear format breaks the essay into manageable pieces for the reader to read and for you to write:
- Introduction: Open with a gripping anecdote, story, or other creative writing technique to draw the reader in. End this paragraph by introducing your themes to be explored.
- 1-3 Body Paragraphs: Explore your themes. Focus on traits that will make you a good physician or otherwise prepare you to excel. Do not tell more stories here, and do not rehash your resume or work and activities section. Introduce activities only to provide context to how they’ve shaped you. Use 2 activities per theme to prove that you possess the skill or trait. Demonstrate that the activities are an expression of yourself, not a simple lesson you learned from an experience.
- Content: To make a personal statement truly unique, you need to look beyond your activities. Write about something you are passionate about. It doesn’t have to be medicine. Some of the greatest residency personal statements I’ve read talk about the lessons they learned in other areas of their life — as a dancer, baseball player, teacher, etc. They connected their learned humility, compassion, perseverance, diligence, patience, and all sorts of characteristics to medicine.
- Conclusion: Wrap it up on a catchy or more emotional note. If the introduction draws the reader in, then the conclusion should leave a lasting impression.
Use AI for editing only, not writing: ChatGPT and similar tools can be helpful during the editing process for your ERAS personal statement. However, don’t let AI do you writing for you. In the first place, it cannot convey the unique stories that make you an attractive candidate. Secondly, admissions committees may be screening applications for AI-generated content.
A good rule of thumb is to only use AI to tweak clunky sentences and improve the overall readability of your statement.
Publications
Here, you will enter information about each publication you’ve been cited in. This is a potentially make-or-break section for highly competitive residencies, so it’s important to work on published research while in medical school if you plan to get into a competitive specialty.
You’ll select publication types from the AAMC’s predetermined list or select “None” if you have no appropriate entries to submit.
Letters of Recommendation
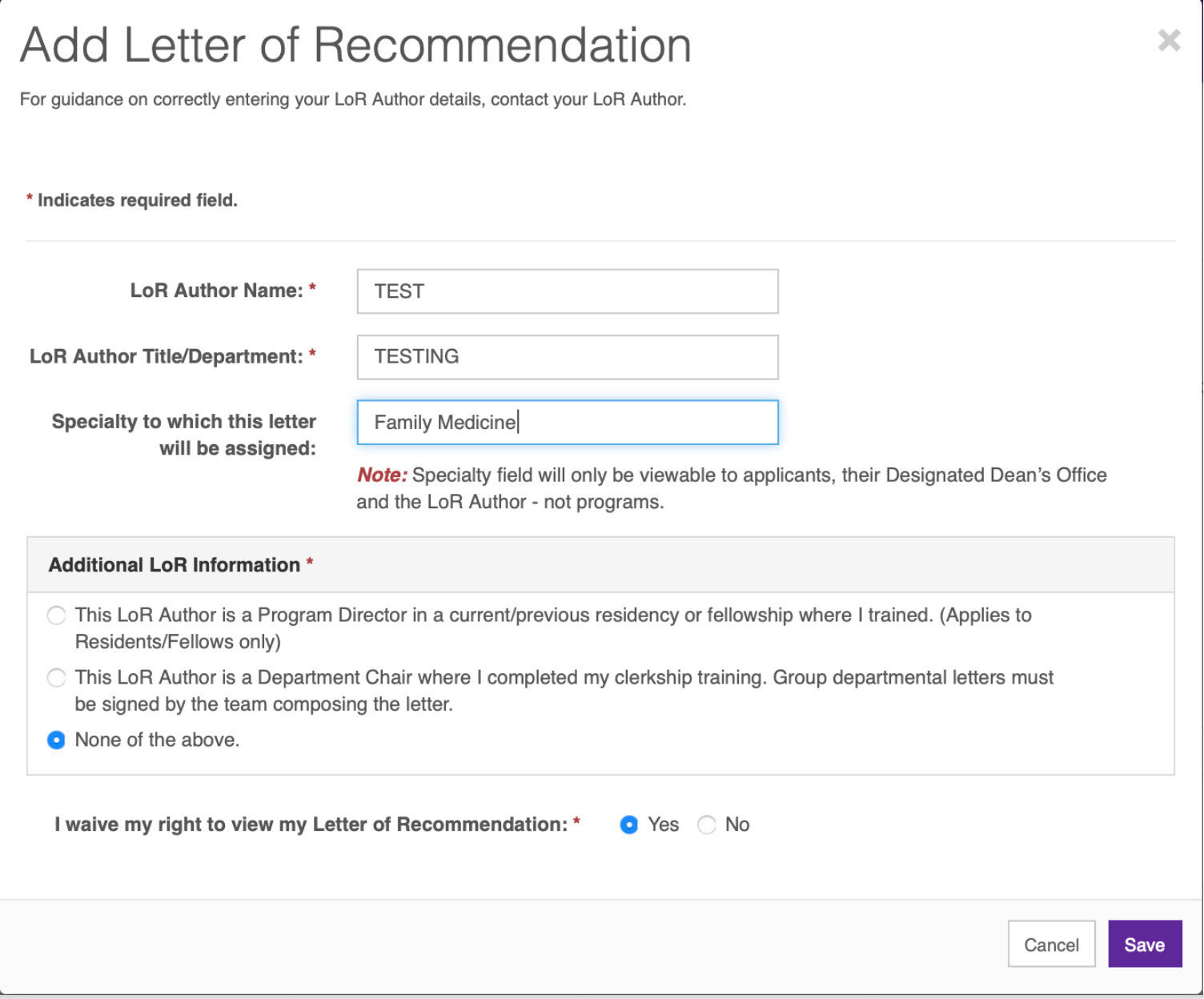
A total of 2-3 letters of recommendation (LORs) from mentors or professional supervisors satisfy most programs’ requirements. Do not wait until right before the application process to request letters.
If you connect with an attending and perform well, ask them if they would be willing to write a letter about 75% of the way through the rotation. Then, ask them for the letter at the end of the rotation.
Collect your letters right away through a 3rd party service like Interfolio so that you can store them ahead of time and upload them when the application process opens.
To use ERAS to request letters, you’ll need to wait until the service opens in June. The applicant has to enter the LOR writer’s name and information and may then generate a letter request form to be sent to the letter writer.
After this step, the applicant must confirm the letter of recommendation.
Once the letter is received in ERAS, then they can assign it to the program of choice.
For more information, the Association of American Medical Colleges has details about the format of the letter. This UCSF page has great information on what to include in the letter.
Medical Student Performance Evaluation (MSPE, or “Dean’s Letter”)
Each school has different policies on how the MSPE process is conducted, so I recommend checking to see if it’s appropriate to contact your Dean about the MSPE. The school will notify the applicant and generate the letter for you to upload to ERAS.
Most schools will automate this with set deadlines from the Dean. Your school will likely require you to attend a meeting before writing the Dean’s Letter/MSPE, where they will require you to present 3 noteworthy characteristics. These will appear in the letter as a bulleted list of no more than 2 sentences each.
Besides Noteworthy Characteristics, other components of the Dean’s Letter/MSPE include:
- Academic history, including info about your matriculation and graduation dates, any leaves of absence, any dual degree programs, any course remediations, and any adverse actions taken against you.
- Academic progress, which includes grades and narrative assessments from courses and clerkships, as well graphical representations of how your performance compares to that of your peers.
- Summary assessment of your performance as a medical student, based on your school’s specific method of evaluation.
- Medical school information, including information about the school’s mission, unusual characteristics, grading system, and how the Dean’s Letter/MSPE is written.
Medical School Transcript
The medical school transcript must be uploaded to ERAS directly from the applicant’s Designated Dean’s Office of their medical school.
ECFMG Status Report (IMGs Only)
This report is for international medical graduates (IMGs) only. The Educational Commission for Foreign Medical Graduates (ECFMG) Status Report verifies the ECFMG Certification status.
The report contains the following information:
- USMLE/ECFMG Identification Number
- Applicant name
- Birth date
- ECFMG-certified: (Yes or No)
- Certificate issue date
- Exams passed for ECFMG Certification
- CSA valid through date, if applicable
- Medical school of graduation
- Degree year
- Medical Education Credential Status (complete or incomplete)
- Explanatory notes (if applicable)
Photograph
You have the option to include a photograph with your application. The photo should be 2.5 x 3.5 inches, with a 150 dpi resolution and a file size of 150KB — or in digital terms, 375 pixels x 525 pixels.
I recommend including a photo. It is the first visual impression the programs will have of you, so make sure you convey the appropriate aesthetic in your photo. I encourage you to invest in a professional headshot. No selfies, please.
USMLE and COMLEX-USA Transcripts
You may upload your USMLE and/or COMLEX transcripts with your application. While this is technically optional, many programs will not consider applicants who do not include these scores. Particularly as Step 1 is now pass/fail for USMLE test-takers, and 90% of residency programs “never” or “seldom” consider students who fail Step 2 on their first take, your board exams are a major factor in your application.
Do I Need to Submit a CV?
You don’t need to create a separate CV apart from your application. The CV compiled in the MyERAS portal is an auto-populated document formatted to include information found elsewhere on your application. If you’d like to have a copy of this document, you can download it by selecting “View/Print CV” in the same area where you can print the entire ERAS application.
ERAS Supplemental Applications Were Removed in 2023
In the past, the AAMC used supplemental applications for residency applicants interested in certain specialties. These supplemental applications included secondary application questions.
ERAS Supplemental Applications were eliminated for the 2023/24 cycle and are not expected to return.
Sample ERAS Personal Statement
Here’s an example of a Personal Statement for your residency application:
"While participating in a high school research program, I examined the stigma women encounter with infertility. The results stunned me. Women felt guilt, embarrassment, and isolation from their inability to conceive. This experience left an indelible impression on me, leading me to pursue a career in women’s health and reproductive function. Throughout my subsequent decade-long involvement with the specialty, I noticed a theme of women exhibiting strength and resilience through their personal challenges and societal constraints. I have chosen to specialize in Obstetrics and Gynecology to improve women’s lives in all circumstances and stages through research, advocacy, and clinical medicine.
As a pre-med undergraduate, I sought to understand what caused infertility by participating in neuroendocrine research regarding hypothalamic-pituitary regulation of ovarian function. I was proud to contribute to our understanding of mechanisms that can potentially be targeted for future therapeutic interventions for women. Throughout my research experience, I refined my practice of returning to the fundamentals when assessing problems and questioning why certain results occur. I intend to continue my research and apply this mindset in residency while troubleshooting disease processes and educating patients on what is happening with their bodies.
In medical school, as I learned about health disparities, I became passionate about patient advocacy and promoting access to care. While serving as a lead for the free gynecology clinic, I learned that many patients missed their appointments because of unreliable transportation, which created a barrier to care. We advocated for free transportation vouchers to remedy this and saw more patients attending their appointments. I plan to be a gynecologist who advocates for patient needs and drives for change because the impact of limited access to care extends far beyond our free clinic--it restricts reproductive rights, increases the public health burden, and leads to poorer outcomes.
My clinical rotations solidified my commitment to pursue OB/GYN. In a particularly poignant moment, I reconnected with a patient during her IUD placement, a year after I first met her during her prenatal appointment. As I admired photos of her new baby, I felt fulfilled by our long connection. Likewise, my gynecologic oncology sub-I exposed me to aspects of surgery that I found fulfilling. I assisted in life-altering cases like a 15-centimeter pelvic mass removal and became so intrigued by rare vulvar pathology that I wrote a case report about it. I was engaged in the technical aspects of gynecological surgery because I enjoy honing my precision and manual dexterity to enhance patient outcomes. Even from my student vantage point as a uterine manipulator, I challenged myself to memorize the steps of the case and tried to anticipate the best maneuvers to assist the primary surgeon. I value the unique blend of developing relationships with women throughout their lifetime and offering surgical solutions that OB/GYN provides. I am a dedicated OB/GYN candidate committed to women's health. My compassion, work ethic, and effective communication skills allow me to connect with patients and deliver patient-centered care. I seek a residency program that values diversity, offers a wide range of surgical exposure, and promotes research. My sub-I experience underlined teamwork in a fast-paced environment, making me keen on programs with collaborative, peer-supported, and mentorship-rich environments. My journey, from research to my sub-internships and my gynecology clinic work, has shown me the resilience of women and their caregivers. I am excited to join this team in advocating and providing compassionate care as a leader in the OB/GYN community."
My recommendation: Try to weave description and content together. Most applicants use a paragraph to tell a story, and then use a sentence or two at the end to reflect on it. This is perfect for a work/activities section, but not for a personal statement. When admissions committee members see this, they start skipping the story and reading the last sentence of each paragraph.
Don’t think activities. Think themes. Think you. Here are some questions to get you thinking about your personal statement:
- What are you great at?
- What are you passionate about?
- What do you like to do?
- What do you have that other applicants don’t have?
- Do you have a unique approach to problem-solving?
- Do you have a unique way of thinking in general?
- Do you have a unique perspective?
- What values are important to you?
ERAS vs. NRMP
It is important to understand that the application process and the matching process are two separate entities: ERAS and NRMP. You’ll need to register for both systems for most residency applications to match.
ERAS allows you to package your application and send it to programs, which in turn will offer you interviews.
NRMP allows you to make and submit a ranked program list from your most to least desirable residency programs. Then, the algorithm matches you. Each year, the NRMP publishes calendars with important dates and deadlines which change by a few days each year. In general, NRMP opens in September, the registration deadline is in November, and rank order lists are due in February.
Choosing a Specialty
Choosing a specialty is very straightforward for some students — you may be so drawn to a single specialty that you choose just one and then fill the rest of the list with “backup specialties.”
For example, Applicant A may be particularly interested in dermatology, so they use a very contiguous list of preferred programs. (The term “contiguous ranks” refers to the number of specialties that appear in a row.)
Applicant A:
- Derm program 1
- Derm program 2
- Derm program 3
- Pediatrics 1
- Pediatrics 2
Other students may have multiple specialty interests and use a non-contiguous list instead.
Applicant B:
- Derm program 1
- Pediatrics 1
- Derm program 2
- Pediatrics 2
- Derm program 3
Both applicants have 3 Derm programs and 2 Pediatrics programs. Applicant A has 3 contiguous ranks for Derm and 2 contiguous ranks for Pediatrics. Applicant B has no contiguous ranks.
The number of contiguous ranks is very important. In 2022, anesthesiology applicants with 11+ contiguous ranks matched with an anesthesiology program 90% of the time. But applicants with only one contiguous rank matched only 45% of the time.
Related: Medical Specialties with Good Work/Life Balance and Low Burnout Rates
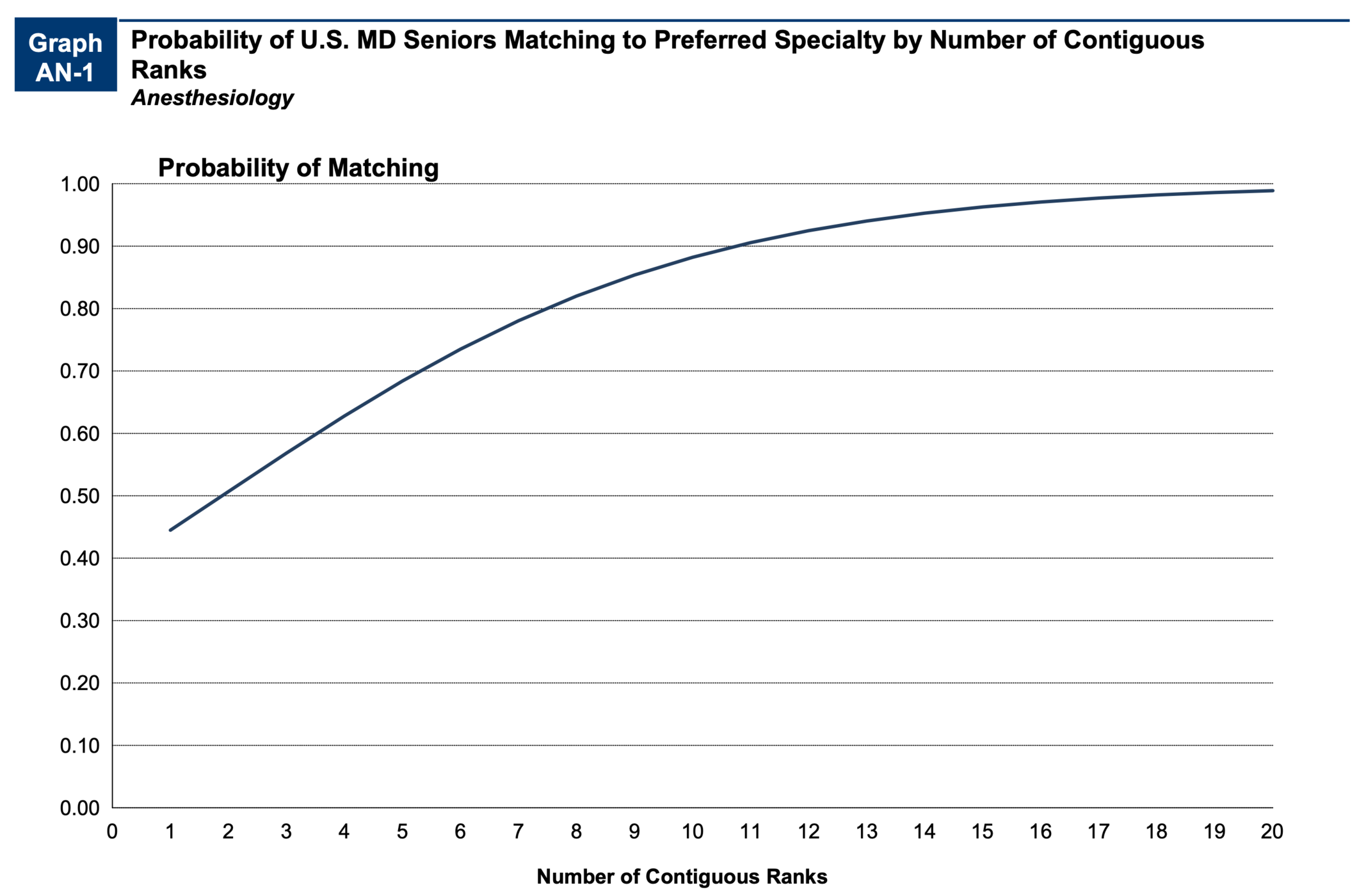
However, you can still rank multiple specialties. The data of previous years has mixed results depending on the specialty. Carefully research the match data about the specialties you’re considering to make a decision on the specialty of choice and how to rank your list accordingly.
What are the odds of matching into residency? In 2024, the odds of matching residency in a first-year position (PGY-1 position) was 80.2%. The match rate into residency of all positions offered was 92.9%. I believe those numbers are slightly down from last year by a percent or two.
Related: Categorical vs. Preliminary vs. Advanced Residency Programs
How Should I Choose a Rank Order List?
Creating a rank order list is straightforward but requires important decision-making. Only rank programs that you would accept an offer from. Rank your most ideal programs at the top.
I strongly suggest reviewing exactly how the matching algorithm works for a better understanding of how to create your rank and list how programs create theirs.
Both the National Resident Matching Program and AAMC have made statements advising applicants to create a rank order list of their true preferences, not how they think they will match.
The final rank order list is due at the end of February to prepare for the match in March.
Residency Interview Questions
Interviews typically start late fall to early winter. I would aim to interview at as many programs as possible. The good news is that since the COVID pandemic, the vast majority of residencies have chosen to conduct their interviews virtually, removing the major financial barrier that was previously in place.
What type of questions are asked during the residency interview? You can expect to find these questions and prompts in a typical residency interview:
- Why did you become a physician?
- What makes you want to be a [specialty]?
- What are your greatest strengths?
- What are your greatest weaknesses?
- Describe a research project you were involved in.
- Name 3 things wrong with the U.S. healthcare system, and propose some fixes.
- What is your interest in this program?
- How do you manage stress?
- What are you looking for in a residency program?
- What do you like to do outside of medicine?
- What other subspecialties did you consider?
- What is the most interesting case you have encountered?
- How would you handle a non-compliant patient?
- What would you do if you saw a senior resident or attending do something wrong?
- Please explain any gaps or discrepancies in your education.
- What elements do you think make a great [specialty]?
- What 3 words would your patients describe you with?
- What 3 words would your colleagues describe you with?
- How would you describe your patient care documentation?
- What’s your approach to developing a rapport with your patients?
- What’s your approach to educating your patients?
- How will you contribute to the diversity of our program?
Worried about your interviews? Prep with former admissions committee members & get live feedback on how to improve your responses!
General Tips on Interview Day
Now you know the sorts of questions you’re gonna get asked. Now let me offer some free tips about your interview day:
- Attire: Dress professionally, and remember, this is not a fashion show. If you happen to be up to date on the newest fashion trends, just remember that your interviewer might not be. Your clothes should be neat and presentable. They should not distract from the content of your message. The same goes for jewelry — try not to wear anything that draws the attention away from your message as a candidate.
- Stature: Sit upright and lean in, just like you would when speaking to a patient. Body language conveys interest, so leaning back with crossed arms will send the wrong message.
- Framing: If you’re participating in a virtual interview, ensure that you look great in the frame by being well-dressed in a brightly-lit area. Make sure that the background behind you appears professional. Having interesting items in your room that are visible on camera can be an excellent conversation starter.
- Ask Questions: Every interview will end with the same question: “What questions do you have for me?” The most common wrong answer is to walk away without asking your interviewer questions. Be prepared with some questions of your own, such as queries about their workplace culture.
- Letter of Intent: Send thank you notes to all interviewers. After you’ve completed your interviews and before you submit your rank order list, send a letter of intent to your top few programs. As the name suggests, these signal your intent to rank the program highly. Note: These are not the same as letters of interest, which are sent prior to interviews.
The Supplemental Offer and Acceptance Program
What is the SOAP program? The SOAP program is designed to fill in the gaps left by the algorithm for applicants that did not get matched. The Monday of Match Week, applicants are notified if they are eligible for SOAP. To be eligible for SOAP, you must be:
- Unmatched
- Registered in the main match through NRMP
- Available to start residency in June
SOAP works in a completely different way than the NRMP. There is no algorithm for SOAP at this time. If you find out you don’t match on Monday of Match week, you obtain access to a list of all unmatched programs through the NRMP website. There, you can select and apply to as many as 45 programs via ERAS.
The programs can call and interview you by phone over the next several days. You are not allowed to contact programs during this time, unless they initiate contact with you. After completing interviews, programs, but not applicants, submit a rank order list of candidates they’ve interviewed.
Based on these lists, SOAP offers are extended on Thursday of Match week. There are four rounds of offers, each lasting for two hours. Round 1 begins at 9 AM ET, round 2 at 12 PM ET, round 3 at 3 PM ET, and round 4 at 6 PM ET.
After receiving an offer in round 1, applicants have two hours to either accept or reject it. Most positions are filled in round 1.
Any applicants who go unmatched in round 1 move on to round 2 and so on until the conclusion of round 4 at 8 PM ET.
Once SOAP ends on Thursday evening, applicants who are still unmatched receive a final list of unfilled programs. Now, the rules change: You may contact the programs on that list and ask for interviews. They can extend an offer to you at any time.
This process is available from Thursday of Match Week until May 1st — about 5 weeks.
All About 3rd & 4th Year Rotations
When should I apply to get matched for residency? You should apply to get matched for residency in the late summer or early fall of your fourth year of medical school.
Before the application process begins, a successful bid for residency requires careful planning of the second half of third-year and the first half of fourth-year. The important parts here are away rotations and use of electives.
Away Rotations (And Free Interviews)
Away rotations are particularly useful for you to find out more about a program, while at the same time, showcasing your talents. These are essentially working interviews, or audition rotations. Away rotations should be chosen based on your interest in matching into one of these locations. As a bonus, you can use them as a required rotation.
When using an away rotation as an elective or a sub-internship rotation (Sub-I), you’ll also get a free interview out of the rotation without having to travel back for another visit. Keep in mind that nearly every school of medicine has time set aside for you to do interviews in your fourth year, so don’t feel compelled to get all your interviews done through away rotations.
In general, I do not recommend doing your first core rotation as an away rotation at a program you’re interested in. If you haven’t done internal medicine yet, don’t show up to an audition rotation for internal medicine. Sure, you’ll learn a ton about the program, but you won’t make a strong impression.
You want to show up to audition rotations at your best, so do a Sub-I or just an elective in that specialty late in your third-year or early in your fourth year.
Timing Your Rotations
Regarding timing, there is no right time to do your audition rotation, but there is a wrong time.
Early in your third year, when you’re not strong clinically, is not the best time. Another time to avoid is when your rank order list is close to being due in February.
The ideal time is anywhere from late Spring of your third year through the end of that calendar year.
How Many Rotations Can I Do?
Practically speaking, you cannot use all your electives and away time to do audition rotations. Your school will have limitations, and you don’t want to spend your whole fourth year doing the same rotations at different hospitals.
Most applicants can afford to do one or two of these and get further exposure to these programs from interviews.
Every school is different, so make sure you sit down with your deans to find out how many aways you can do, when you can do them, what specialties you can do them with, and how much time is set aside for electives.
Read Next: Is a 3-Year Medical School Right for You?
Important Note for International Students
International medical graduates (IMGs) are inherently at a disadvantage compared to American medical graduates (AMGs) for multiple reasons. What determines you being an IMG is whether you attend or graduated from a medical school outside the USA or Canada — not where you were born.
Note: For medical school graduates in the class of 2026 and beyond, Canada and the USA will no longer practice reciprocity and will consider graduates of the other country as IMGs.
Most program directors are familiar with and confident about the medical education AMGs receive. However, many programs view IMGs as somewhat of an unknown, as they already have a large pool of applicants applying for a smaller group of positions, and international medical schools have widely varied standards.
IMGs need to show more competitiveness. That means higher USMLE scores, more research, and more volunteer activities — anything that helps give you an edge when applying. Other than that, all the same principles for a successful application apply to a non-US med student as to a US med student.
One particularly important note is selecting IMG-friendly states. I suggest looking at the data to identify programs that tend to accept IMGs and avoid highly ranking programs that have a history of not accepting them.
Once you’ve identified which states match IMGs into the specialty of your choice, the next step is to look at the Residency Explorer tool to specifically find out how many IMGs match into specific programs.
Read Next: What Are MD-PhD Programs? Overview & Program List
Stay Ahead of the Curve. Increase Your Chances.
The residency application process is a long road requiring ample planning. What’s more, close to 20% of applicants don’t end up matching into a PGY-1 position. So stay ahead of the curve by investing in 1-on-1 mentorship throughout the application process, from carefully selected audition rotations all the way to Match Day.
Work 1-on-1 with a Match Advisor & join the 97% of MedSchoolCoach clients who match into residency!

Amar Mandalia, MD
Dr. Mandalia is an accomplished medical writer with multiple manuscripts in peer-reviewed journals and a practicing GI physician in the Orlando area. He is the Admissions Advisor for MedSchoolCoach and has extensive experience helping students get into medical school and residency.